How Is A Hill Sachs Lesion Repair Orthoscope
- Enquiry article
- Open Access
- Published:
Outcomes of arthroscopic "Remplissage": capsulotenodesis of the engaging large Hill-Sachs lesion
Journal of Orthopaedic Surgery and Enquiry volume 6, Article number:29 (2011) Cite this article
Abstract
Groundwork
A Loma-Sachs lesion of the humeral caput after a shoulder dislocation is clinically insignificant in almost cases. However, a sizable defect will engage with the anterior rim of the glenoid and cause instability fifty-fifty subsequently anterior glenoid reconstruction. The purpose of this study was to evaluate the outcome of arthroscopic capsulotenodesis of the posterior capsule and infraspinatus tendon ("remplissage") to seal a big engaging Hill-Sachs lesion in an unstable shoulder.
Methods
This was a prospective follow-up study of patients who underwent arthroscopic surgery for recurrent shoulder instability with a large engaging Hill-Sachs lesion from 2007 to 2009. The clinical results were measured preoperatively and postoperatively with the Unproblematic Shoulder test (SST) and the Rowe score for instability.
Results
Eleven patients met the inclusion criteria of this study. The mean follow-upwardly time was 30 months (range 24 to 35 months). At the last follow-up, meaning improvement was observed in both scores with no recurrent dislocations. The hateful SST improved from six.half dozen to eleven (p < 0.001). The hateful Rowe Score improved from 10.half dozen to 85 points (p < 0.001). On boilerplate patients regained more than than 80% of shoulder external rotation.
Conclusions
Arthroscopic remplissage for shoulder instability is an effective soft tissue technique to seal a large engaging Hill-Sachs lesion with respect to recurrence charge per unit, range of motion and shoulder role.
Introduction
Posterior-lateral compression fracture of the humeral head (a Hill-Sachs lesion) is a common finding associated with anterior shoulder instability [i–3]. Virtually Loma-Sachs lesions are clinically insignificant and practice not crave surgical treatment. Still, Palmer and Widen [4] realized that a sizable defect volition engage with the anterior rim of the glenoid and cause instability even after anterior glenoid reconstruction. The term engaging Hill-Sachs lesion was used by Burkhart and De Beer [5] to describe the leverage of the humeral head from the glenoid rim in the presence of a large bony defect. They concluded that arthroscopic stabilization in the presence of such bony deficiencies is likely to fail and requires open surgery. Thus, despite an adequate Bankart repair, consideration must be given toward treating the associated posterolateral defect inside the humeral head if it is of sufficient size. Several unlike reconstructive solutions have been proposed for dealing with large Hill-Sachs lesions. These solutions vary from soft tissue transfers [6] to bony reconstructions such as humeral osteotomy [7], structural osteochondral allografts [8] and transhumeral impaction grafting [9]. Others advocate hemi arthroplasty [x] as a definitive treatment. Recently, Purchase et al [11] presented a technique of capsulotenodesis of the posterior sheathing and infraspinatus tendon to fill up the Hill-Sachs lesion tendon (also known as the French term "remplissage"). The purpose of our study was to evaluate the upshot of arthroscopic remplissage in an unstable shoulder with a large engaging Hill-Sachs lesion. Our hypothesis was that arthroscopic remplissage is an effective offshoot to shoulder stabilization in the presence of engaging Hill-Sachs lesions in terms of part and patient satisfaction.
Materials and methods
Overall, 65 all arthroscopic shoulder stabilizations were performed in our institution from 2007 to 2009. Up to date, 25 patients were identified in whom arthroscopic shoulder stabilization included a capsulotenodesis to fill the humeral head lesion in add-on to capsulolabral repair around the glenoid rim. This procedure was done in patients without a significant glenoid bone loss. This written report included patients with a minimum follow-upwards of 2 years (eleven of the 25 patients). The diagnosis of recurrent, inductive shoulder instability was made on the basis of a history of recurrent anteroinferior dislocation or subluxation with physical signs of anteroinferior instability. All patients underwent preoperative radiographic and MRI evaluations. The conclusion to accost the lesion was made during arthroscopy if the posterolateral humeral defect engaged the inductive rim of the glenoid in abduction and external rotation of less than xc°, every bit described Koo et al [12]. Data was retrieved from the surgical reports and follow-up files.
All patients provided formal informed consent for participation in this study.
With a mean follow-up time of xxx months (range 24 to 35) evaluations were performed pre and post operatively by an contained observer co-ordinate to the shoulder rating scales of Rowe et al [xiii] and the Uncomplicated Shoulder Examination (SST) [fourteen]. Table 1 shows patient demographics.
All arthroscopies were done by a single surgeon experienced in that procedure. Every operation started with an exam under general anesthesia. Anteroposterior humeral translation was examined with the patient'due south arm in xc° of abduction and varying degrees of external rotation. The translation was rated equally course 0 (no translation), grade 1+ (translation of less than the margin of the glenoid), class 2+ (translation across the margin of the glenoid with spontaneous reduction), or grade 3+ (translation beyond the glenoid without spontaneous reduction). Junior translation was measured according to the subacromial sulcus sign. The distance between the inferior margin of the lateral aspect of the acromion and the humeral head was measured and was rated as class 0 (no sulcus), grade 1 (<1 cm), form 2 (1 to 2 cm), or class 3 (>2 cm). In principle, nosotros used a similar surgical technique of the Hill-Sachs remplissage already described past Purchase et al [xi]. Briefly, the surgery was performed nether combined general anesthesia and interscalene block. The patient was placed in the lateral decubitus position on a beanbag support to tilt the torso approximately 20° posteriorly with the arm in fifty° abduction, 20° flexion and five kg of traction. Initially a posterior portal was created then anterosuperior, and anteroinferior portals penetrating the superior and junior borders of the rotator interval, respectively. The antroinferior portal was the main working portal for inductive labral repair and the remplissage was done through the posterior portal. Diagnostic arthroscopy was performed through the posterior and anterosuperior viewing portals. Subsequently evaluating the capsulolabral damage, the arm was temporarily released from traction and the scope was aimed to the Hill-Sachs lesion while dynamic exam in abduction and external rotation was performed under visualization (Effigy 1A). If an engaging Loma-Sachs lesion was found in the position of abduction and external rotation of less than xc°, one or 2 anchors (LUPINE™ BR Anchor w/#two ORTHOCORD®, DePuy Mitec Inc.) were inserted into the Hill-Sachs lesion via the posterior portal. The suture limbs were left untied at that stage (Figure. 1B). The anterior capsulolabral repair was and then performed. Finally, the remplissage was performed while viewing from the anterosuperior portal. The posterior cannula was withdrawn posterior to the capsule and infraspinatus into the subdeltoid space. A penetrating grasper (Figure 1C) was used to retrograde the sutures through the adjacent posterior capsule. This was done superior and inferior to the initial portal entry site. The sutures were and then tied blind in the subdeltoid space.
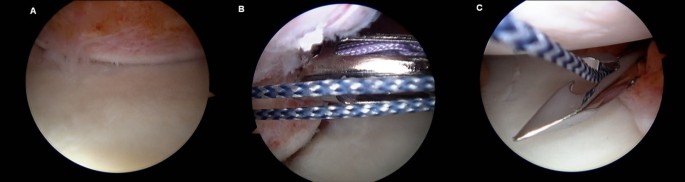
Images illustrate arthroscopic remplissage . (A) An engaging Colina-Sachs lesion. (B) Anchors are inserted into the humeral caput defect. (C) A penetrating grasper is used to retrograde the sutures through the next posterior capsule.
Post operatively the shoulder was protected in a sling for four weeks while performing movements of elbow, wrist and fingers. At week three the patient started isometric exercises and at week 4 shoulder external rotation motion. After week 4 the patient was encouraged to perform superlative above 90° and was reviewed by the surgeon and physiotherapist at 6 weeks afterwards the surgery. During weeks 6 to 12 the patient gradually increased elevation and rotation strengthening exercises. Render to sport was immune later six months when at to the lowest degree xc% of shoulder strength and range of motion had been regained.
Results were expressed with descriptive methods (hateful, range). The paired Educatee'southward t exam was used for comparison between scores before and subsequently surgery. P value of less than 0.05 was considered statistically significant.
Results
There were no recurrent dislocations and no patient had further surgery on his shoulder. At the fourth dimension of the follow-up all patients had returned to their regular jobs and normal activities including the 2 athletes who had returned to play on professional level. All patients had a large engaging Hill-Sachs lesion which was treated by a remplissage utilizing 1 or two anchors into the humeral head defect. Boosted common surgical findings are presented in Table 2. None of the patients had a rotator interval closure.
Overall, the average number of positive responses on the 12-question Uncomplicated Shoulder Exam were 6.vi before the operation and 11 at the last follow-up (p < 0.001). The Rowe score for instability improved from 10.6 preoperatively to 85 at the last follow-upwards (p < 0.001) and was considered practiced to excellent in 78% of the patients (Table 3). While mail service operative acme and internal rotation motions were documented every bit normal, external rotation motility was found to exist limited to an boilerplate of 83% of the range that was plant in the contralateral shoulder. There were no postoperative complications.
Discussion
Our findings suggest that performing the remplissage technique in conjunction with Bankart repair on unstable shoulders with large engaging Hill-Sachs lesion provides good short term functional results with no recurrent dislocations.
The presence of a large Loma-Sachs lesion can engage with the anterior glenoid rim with the arm in abduction and external rotation levering the humeral head anteriorly. This mechanism has been regarded as a significant crusade of recurrent shoulder dislocations and of arthroscopic reconstruction failure [5]. The handling of osseous defects as part of shoulder stabilization surgery was recently reviewed by Bushnell et al [xv] and Lynch et al [16]. Specifically, humeral head defects can exist addressed in several ways. The defect tin exist redirected using the Weber rotational osteotomy [7] to increase the retroversion of the proximal humerus. All the same, although the published results were good [17] most patients had an internal rotation deficit and there is a considerable risk of malunion or nonunion. Other options are to seal the defect with structural allograft [8] or transhumeral impaction bone grafting [9]. The former requires an all-encompassing open arroyo with risks of graft or hardware failure while the afterward is less invasive and more anatomical but might not exist suitable for large defects or osteopenic patients. Recently, Chapovsky and Kelly described an all-arthroscopic technique to make full the defect with an osteoarticular allograft [xviii]. A Prosthetic resurfacing arthroplasty has also been used to care for focal deficits of the humeral head [xix, 20] but since shoulder instability is mostly encountered in the younger population with a higher likelihood of prosthetic failure it is a less favorable solution. From 2007 the senior author has started to use the remplissage technique for instability cases involving a large posterior engaging Colina-Sachs lesion. The decision to perform a remplissage was made during arthroscopy. The all arthroscopic technique was previously described by Wolf and colleagues for handling of combined glenoid loss and a Colina-Sachs lesion [eleven] and also by Krackhardt et al [6] for a reverse Loma-Sachs lesion. The principle is a fixation of the conjoined infraspinatus tendon and posterior capsule to the abraded surface of the humeral head defect. At the 26th Almanac Meeting of the Arthroscopy Association of North America, Wolf et al reported on an unpublished study of 24 patients with a minimum of 2-year follow-up. Xx two were very satisfied; of these, 15 reported excellent results and seven had good results. Ii patients were rated with poor results. The 8 patients in whom prior surgery had failed were without recurrence at follow-upwardly. There were two recurrent dislocations, one due to a motorcycle blow and the other resulting from a wrestling lucifer. They ended that "Filling the lesion effectively obliterates the Hill-Sachs lesion and converts it into an extra-articular lesion, thereby preventing appointment. There were no significant complications, and the business that the remplissage would limit rotation did not materialize". The patients in our study were mostly a community-based young population merely too included two professional athletes (Australian Football game players). In our electric current study the results showed a significant comeback at the last follow-up (mean 30 months) with no recurrent dislocations. We used the Elementary Shoulder Test which was previously found reliable, valid and responsive [14] to document functional improvement. Overall, the average number of positive responses on the 12-question Simple Shoulder Test were 6.vi before the functioning and xi at the last follow-upwardly (p < 0.001). We used the Rowe score [13] to assess postoperative stability. The Rowe score for instability improved from 10.6 preoperatively to 85 at the last follow-up (p < 0.001) and was considered skilful to first-class in 78% of the patients postoperatively.
We share the opinion of Koo et al. [12] on this procedure's advantages. It is a minimally invasive approach to catechumen an intra-articular lesion into an actress-articular lesion, without the morbidity associated with open procedures and no additional graft fabric, thereby making the procedure quick and easy to perform.
Even though in that location is a business organization that the tenodesed cuff and capsular tissue tin can human action every bit a mechanical block to external rotation of the shoulder [21] it was found to be minor in our patients and did not interfere with daily activities.
The strength of this study is in its uniform surgical indication, operative technique, postoperative care and follow-upwardly methodology. Nevertheless it has several limitations. Offset, all procedures were performed by the aforementioned surgeon which might non reverberate other people's results. Another drawback is the small number of patients (most participate in recreational sports only) and the relative short follow-upwards time. This is considering the technique was introduced but recently and significant Hill-Sachs lesions are relatively rare. Thus in order to support our results there is a need for long term controlled studies preferably with a larger accomplice of patients.
Conclusions
Arthroscopic remplissage for shoulder instability offers an constructive soft tissue technique to seal a large engaging Loma-Sachs lesion with respect to recurrence charge per unit, range of motion and shoulder function.
References
-
Yiannakopoulos CK, Mataragas East, Antonogiannakis E: A comparison of the spectrum of intra-articular lesions in acute and chronic inductive shoulder instability. Arthroscopy. 2007, 23 (9): 985-990. 10.1016/j.arthro.2007.05.009.
-
Spatschil A, Landsiedl F, Anderl West, Imhoff A, Seiler H, Vassilev I, Klein W, Boszotta H, Hoffmann F, Rupp S: Posttraumatic anterior inferior instability of the shoulder: arthroscopic findings and clinical correlations. Arch Orthop Trauma Surg. 2006, 126 (4): 217-222. 10.1007/s00402-005-0006-4.
-
Calandra JJ, Baker CL, Uribe J: The incidence of Colina-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy. 1989, 5 (4): 254-257. 10.1016/0749-8063(89)90138-two.
-
Palmer I, Widen A: The bone block method for recurrent dislocation of the shoulder joint. J Bone Articulation Surg Br. 1948, 30: 53-58.
-
Burkhart SS, De Beer JFB: Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000, xvi: 677-694. 10.1053/jars.2000.17715.
-
Krackhardt T, Schewe B, Albrecht D, Weise Grand: Arthroscopic fixation of the subscapularis tendon in the reverse Hill-Sachs lesion for traumatic unidirectional posterior dislocation of the shoulder. Arthroscopy. 2006, 22 (2): 227.e1-227.e6. x.1016/j.arthro.2005.x.004.
-
Weber BG, Simpson LA, Hardegger F: Rotational humeral osteotomy for recurrent inductive dislocation of the shoulder associated with a big Hill-Sachs lesion. J Bone Joint Surg Am. 1984, 66: 1443-1450.
-
Miniaci A, Berlet G: Recurrent anterior instability following failed surgical repair: Allograft reconstruction of large humeral head defects. J Os Joint Surg Br. 2001, 83 (Suppl 1): 19-20.
-
Kazel MD, Sekiya JK, Greene JA, Bruker CT: Percutaneous correction (humeroplasty) of humeral head defects (Colina-Sachs) associated with anterior shoulder instability: a cadaveric written report. Arthroscopy. 2005, 12: 1473-1478.
-
Moros C, Ahmad CS: Fractional humeral head resurfacing and Latarjet coracoid transfer for treatment of recurrent anterior glenohumeral instability. Orthopedics. 2009, 32 (8):
-
Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC: Hill-sachs "remplissage": an arthroscopic solution for the engaging colina-sachs lesion. Arthroscopy. 2008, 24 (6): 723-726. 10.1016/j.arthro.2008.03.015.
-
Koo SS, Burkhart SS, Ochoa Eastward: Arthroscopic double-pulley remplissage technique for engaging Hill-Sachs lesions in inductive shoulder instability repairs. Arthroscopy. 2009, 25 (11): 1343-1348. 10.1016/j.arthro.2009.06.011.
-
Rowe CR, Patel D, Southmayd WW: The Bankart procedure: a long-term terminate-result study. J Bone Joint Surg Am. 1978, threescore: 1-16.
-
Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher 1000: Reliability, validity, and responsiveness of the simple shoulder exam: psychometric backdrop by age and injury type. J Shoulder Elbow Surg. 2007, 16 (3): 260-267. ten.1016/j.jse.2006.07.003.
-
Bushnell BD, Creighton RA, Herring MM: Bony instability of the shoulder. Arthroscopy. 2008, 24 (ix): 1061-1073. 10.1016/j.arthro.2008.05.015.
-
Lynch JR, Clinton JM, Dewing CB, Warme WJ, Matsen FA: Treatment of osseous defects associated with anterior shoulder instability. J Shoulder Elbow Surg. 2009, 18 (ii): 317-328. 10.1016/j.jse.2008.10.013.
-
Kronberg M, Brostrom LA: Rotation osteotomy of the proximal humerus to stabilise the shoulder. Five years' feel. J Os Joint Surg Br. 1995, 77: 924-927.
-
Chapovsky F, Kelly JDIV: Osteochondral allograft transplantation for treatment of glenohumeral instability. Arthroscopy. 2005, 21: 1007-
-
Scalise JJ, Miniaci A, Iannotti JP: Resurfacing arthroplasty of the humerus: Indications, surgical technique, and clinical results. Tech Shoulder Elbow Surg. 2007, viii: 152-160. 10.1097/bte.0b013e31806196e6.
-
Raiss P, Aldinger PR, Kasten P, Rickert M, Loew M: Humeral head resurfacing for fixed anterior glenohumeral dislocation. Int Orthop. 2009, 33 (two): 451-456. 10.1007/s00264-007-0487-6.
-
Deutsch AA, Kroll DG: Decreased range of motility following arthroscopic remplissage. Orthopedics. 2008, 31 (5): 492-
Author information
Affiliations
Respective author
Boosted information
Competing interests
The authors declare that they accept no competing interests.
Authors' contributions
All authors had substantial contributions in following up the patients and in data collection. DB has performed the surgeries. BH and LM have assisted in surgeries. BH participated in the design of the study and performed the statistical assay. DB conceived of the study, and participated in its design and coordination. All authors read and approved the last manuscript.
Authors' original submitted files for images
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Admission article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and Permissions
Almost this article
Cite this commodity
Haviv, B., Mayo, L. & Biggs, D. Outcomes of arthroscopic "Remplissage": capsulotenodesis of the engaging large Colina-Sachs lesion. J Orthop Surg Res half dozen, 29 (2011). https://doi.org/10.1186/1749-799X-half-dozen-29
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1186/1749-799X-6-29
Keywords
- Humeral Head
- Shoulder Instability
- Recurrent Dislocation
- Anterior Shoulder Instability
- Unproblematic Shoulder Exam
Source: https://josr-online.biomedcentral.com/articles/10.1186/1749-799X-6-29
Posted by: faustsace1973.blogspot.com


0 Response to "How Is A Hill Sachs Lesion Repair Orthoscope"
Post a Comment